- SHOP
- LEARN
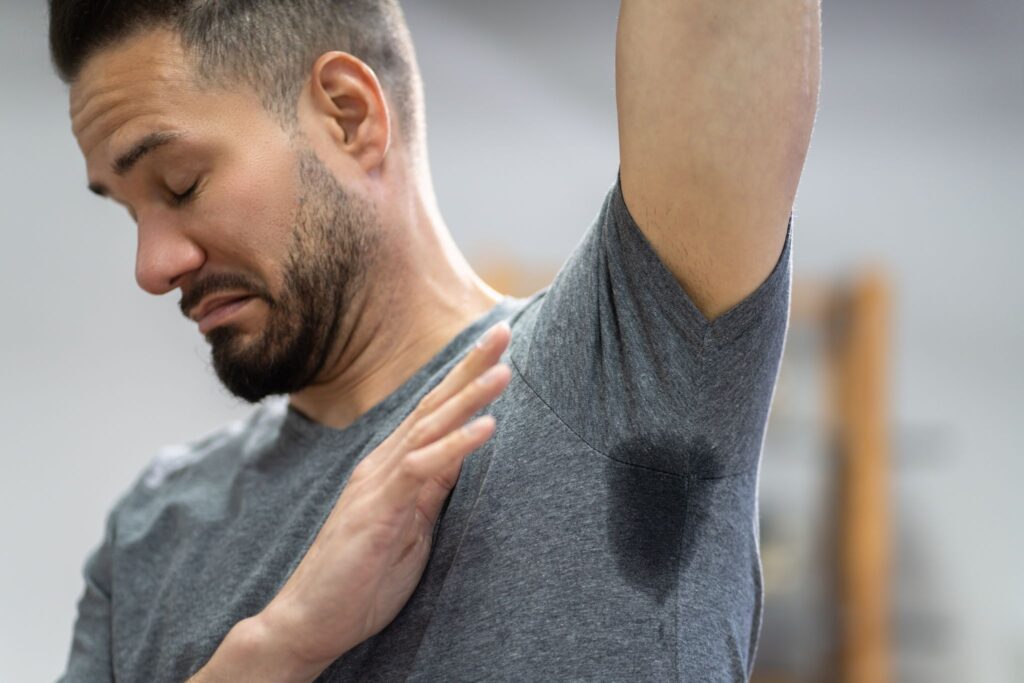
- How to stop sweating
The ultimate guide to stopping sweat
Sweating too much?Learn why you might be sweating more than normal
-
- FAQs
- ABOUT
- SHOP
- LEARN
- How to stop sweating
The ultimate guide to stopping sweat
Sweating too much?Learn why you might be sweating more than normal
-
- FAQs
- ABOUT